Importance of healthcare sector & its inter-linkages with economic sectors
"It is health that is real wealth and not pieces of gold and silver.”
—Mohandas K. Gandhi
|
"It is health that is real wealth and not pieces of gold and silver.” —Mohandas K. Gandhi |
Introduction:
- The recent COVID-19 pandemic has emphasized the importance of the healthcare sector and its inter-linkages with other key sector of the economy.
- The ongoing pandemic has showcased how a healthcare crisis can get transformed into an economic and social crisis.
- Given its potential to provide healthcare access in remote areas, telemedicine needs to be harnessed to the fullest by especially investing in internet connectivity and health infrastructure.
- As a bulk of the healthcare in India is provided by the private sector, it is critical for policymakers to design policies that mitigate information asymmetry in healthcare, which creates market failures and thereby renders unregulated private healthcare sub-optimal.
- Increased prioritization of healthcare in the central and state budgets is important as it crucially impacts how much protection citizens get against financial hardships due to out of- pocket payments made for healthcare.
Covid-19 and India’s health care policy
- Following the Covid-19 pandemic, a key portfolio decision that healthcare policy must make is about the relative importance placed on communicable versus non-communicable diseases.
- As pandemics represent rare events, healthcare policy can become a victim of “saliency bias”, which involves over-weighting recent phenomena.
- 71 per cent of global deaths and about 65 per cent of deaths in India are caused by non-communicable diseases.
- Further, preventing communicable diseases requires focus on better sanitation and drinking water, which the Swachh Bharat and the Har Ghar Jal Abhiyan campaigns are focusing on.
What are the issues with Indian Healthcare system?
- Despite improvements in healthcare access and quality (healthcare access and quality scored at 41.2 in 2016, up from 24.7 in 1990), India continues to underperform in comparison to other Low and Lower Middle Income (LMIC) countries.
- On quality and access of healthcare, India was ranked 145th out of 180 countries (Global Burden of Disease Study 2016).
- Only few sub-Saharan countries, some pacific islands, Nepal and Pakistan were ranked below India.
Poor health outcomes
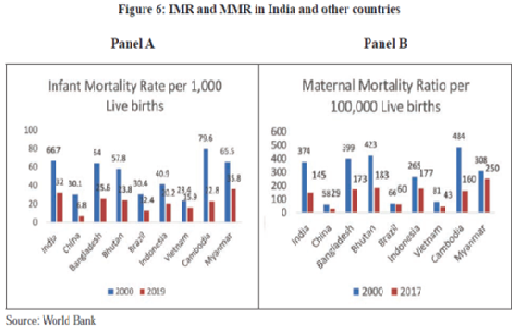
- As seen in figure despite improvements in MMR and IMR, India still needs to improve significantly on these metrics.
- Countries such as China, Bangladesh, Bhutan, Cambodia, etc. have improved much more on these metrics than India.
Low access and utilisation
- At 3-4 per cent, the hospitalisation rates in India are among the lowest in the world; the average for middle income countries is 8-9 per cent and 13-17 per cent for OECD countries (OECD Statistics).
- The low hospitalisation rates reflect lower access and utilisation of healthcare in India.
Inequality in health care
- Though decreasing in recent years, inequity persists in availability of healthcare.
- In recent times, the percentage of the poorest utilising prenatal care through public facilities has increased from 19.9 per cent to 24.7 per cent from 2004 to 2018, and there is a similar increase in the percentage of the poor accessing institutional delivery as well as post-natal care.
Low budget allocations for healthcare
- As health is a state subject in India, spending on healthcare by states matters the most when examining government healthcare spending. According to National Health Accounts, 2017, 66 per cent of spending on healthcare is done by the states.
- India ranks 179th out of 189 countries in prioritization accorded to health in its government budgets (consolidated union & state government).
Low public health expenditure as compared to other countries
- An increase in public health expenditure from the current levels in India to 3 per cent of GDP can reduce the OOP expenditure from 60 per cent currently to about 30 per cent.
- Increased prioritization of healthcare in the central and state budgets is important as it crucially impacts how much protection citizens get against financial hardships due to outof- pocket payments made for healthcare.
- OOP for health increase the risk of vulnerable groups slipping into poverty because of catastrophic health expenditures.
The state expenditure on healthcare highly variable across states
- The state expenditure on healthcare is highly variable across states and is not fully explained by the income level of the state.
- While healthcare spending per capita increases with the GSDP per capita, healthcare spending as a per cent of GSDP decreases with the GSDP per capita. Thus, the richer states are spending a lower proportion of their GSDP on healthcare.
- The states that have higher per capita spending have lower out-of-pocket expenditure, which also holds true at global level.
Low human resources for health
- World Health Organization (WHO) identified an aggregate density of health workers to be 44.5 per 10,000 population and an adequate skill-mix of health workers to achieve composite SDG tracer indicators index by 2030.
- The WHO also specified a lower range of 23 health workers per 10,000 population to achieve 80 per cent of births attended by skilled health professionals.
- Although aggregate human resources for health density in India is close to the lower threshold of 23, the distribution of health workforce across states is lop-sided.
Unregulated private enterprise in an industry marked by high level of market failure
- While the share of public institutions has increased both in hospital and outpatient cares, the private sector dominates in total healthcare provision in India.
- Around 74 per cent of outpatient care and 65 per cent of hospitalisation care is provided through the private sector in urban India.
What are the inherent characteristics of healthcare system?
Healthcare systems do not self-organise using the force of free markets because of three key inherent and unchanging characteristics:
- Uncertainty/variability of demand;
- Information asymmetry; and
- Hyperbolic tendencies.
Hence, any active system design of healthcare must be mindful of these inherent characteristics.
Need for system design in healthcare
- Most well-functioning health systems are structured as oligopolies purchasing from oligopsonys instead of individual consumers purchasing from individual providers.
- The structure of the market has substantial implications for long term trajectory of the health system.
- Countries with more fragmented health systems tend to have lower performance as reflected in higher costs, lower efficiency, and poor quality.
- Therefore, in addition to providing healthcare services and financing healthcare, a key role for the government is to actively shape the structure of the healthcare market.
International Experience in Regulating Healthcare
Australia
- National Safety and Quality Health Service (NSQHS) Standards developed by the Australian Commission on Safety and Quality in Health Care (ACSQHC) are part of the Australian Health Services Safety and Quality Accreditation Scheme endorsed by the Australian health ministers in 2010.
England
- Following the 2012 Health and Social Care Act, the NHS in England has undergone considerable change, with reform implementation continuing. In addition to regulators professional statutory bodies also have an important role in England.
- Currently, they use a mix of enforcement and punishment to ensure compliance.
Finland
- The Finnish Constitution sets out the requirement that government must provide adequate care for all, providing the legal foundation for national regulation such as the 1992 Act on the Status and Rights of Patients.
Netherlands
- The Dutch government has defined quality of care in terms of effectiveness (clinical effectiveness; patient safety), patient centeredness and cost-efficiency, which form the basis of the regulatory system and national regulation.
USA
- The 2010 Affordable Care Act required the Department of Health and Human Services (DHHS) to develop a National Strategy for the Improvement of Heath Care (National Quality strategy). The Nursing Home Reform act (OBRA’87) deals with nursing home regulation.
- The National Quality Strategy is a developing strategy guided by DHHS as an attempt to set national aims and priorities in healthcare quality improvement. The strategy has three aims: better care, healthy people and communities, and affordable care.
- The OBRA’87 deals with nursing home regulation; it defines regulatory standards for nursing homes at the federal level, supplemented by individual state laws.
Telemedicine
- Impressive growth has been seen in the adoption of telemedicine in India since the outbreak of the COVID-19 pandemic. This coincided with the imposition of lockdown in India and the issuance of the Telemedicine Practice Guidelines 2020 by the Ministry of Health and Family Welfare (MoHFW) on March 25, 2020.
- eSanjeevani OPD (a patient-to-doctor tele-consultation system) has recorded almost a million consultations since its launch in April 2020.
- The success of telemedicine critically hinges on having decent level of health infrastructure and Internet connectivity nationwide.
- Specifically, investing in Internet access, can lead to greater uptake of telemedicine, which in turn can greatly help reduce geographic disparities in healthcare access and utilization.
Way forward:
Long-term healthcare priorities
- Countries with much higher healthcare investments and concomitant health infrastructure have struggled to contain the pandemic. The next health crisis may not possibly involve a communicable disease. Therefore, India’s healthcare policy must continue focusing on its long-term healthcare priorities.
- Simultaneously, to enable India to respond to pandemics, the health infrastructure must be agile. For instance, every hospital may be equipped so that at least one ward in the hospital can be quickly modified to respond to a national health emergency while caring for the normal diseases in usual times.
Role of technology-enabled platforms
- The ongoing COVID-19 pandemic has helped showcase the role of technology-enabled platforms as an alternate distribution channel for remote delivery of healthcare services.
- These technology-enabled platforms offer a promising new avenue to address India’s last-mile healthcare access and delivery challenges. These technology platforms coupled with digitization and the promise of artificial intelligence at-scale, have led to a drastic uptake in the utilisation of telemedicine for primary care and mental health.
- Given India’s unique last mile challenges, such technology-enabled solutions need to be harnessed to the fullest. As we show, telemedicine depends crucially on internet connectivity and health infrastructure.
- Therefore, both Central and the State governments need to invest in telemedicine on a mission mode to complement the government’s digital health mission and thereby enable greater access to the masses.
Role of the National Health mission
- The National Health mission has played a critical role in mitigating inequity in healthcare access. The percentage of the poorest utilising prenatal care through public facilities has increased from 19.9 per cent to 24.7 per cent from 2004 to 2018.
- Similarly, the percentage of the poorest accessing institutional delivery increased from 18.6 per cent to 23.1 per cent and from 24.7 per cent to 25.4 per cent for post-natal care.
- The poorest utilising inpatient care and outpatient care has increased from 12.7 per cent to 18.5 per cent and from 15.6 per cent to 18.3 per cent. Therefore in conjunction with Ayushman Bharat, the emphasis on NHM should continue.
Health Insurance
- With limited visibility into patients’ medical records and no standardised treatment protocols, insurance companies have a risk of adverse selection at the time of policy issuance and a risk of moral hazard at the time of claims.
- To safeguard against this risks, insurance companies resort to high premiums and restriction of services covered in the insurance policy.
- Addressing this information asymmetry can help lower premiums, enable the offering of better products and help increase the insurance penetration in the country